Cuboid Syndrome is a Lesser-Known Foot Condition

Cuboid syndrome, though less common than other foot ailments, can cause significant discomfort and impairment in affected individuals. This condition occurs when the cuboid bone, located on the outer side of the foot, becomes displaced from its normal position within the foot's arch. The exact cause of cuboid syndrome is often attributed to overuse or repetitive stress, such as excessive running, jumping, or wearing poorly fitting shoes. Symptoms of cuboid syndrome typically include pain and tenderness along the outer edge of the foot, difficulty in walking or bearing weight, and limited range of motion in the ankle and midfoot. While cuboid syndrome is considered a rare injury, it is important to seek prompt medical attention if suspected, as delayed diagnosis and treatment can lead to prolonged discomfort and complications. Treatment options for cuboid syndrome may include rest, orthotics, and in severe cases, manipulation or mobilization techniques performed by a podiatrist to realign the cuboid bone and restore proper foot function. If you have pain in this part of your foot, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and treatment.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Cuboid Syndrome
Though cuboid syndrome predominately affects athletes, non-athletes can suffer from it too. Cuboid syndrome is also called cuboid subluxation or cuboid fault syndrome, and occurs when a joint or ligament near the cuboid bone of the foot becomes damaged, or when the bone itself is dislodged from its natural position. Pain may be persistent, or come and go, and it is usually marked by the outside of the foot. Cuboid syndrome, unless severe, can be difficult to diagnose. A doctor will likely ask questions about how long the pain has been present, and will apply pressure on the cuboid bone to determine the origin of pain.
There are a number of causes that can lead to the syndrome. Due to athletic activities, repeated stress placed on the foot can cause cuboid subluxation. Ballet dancers, runners, and other athletes often develop this condition. Basketball or tennis players may also develop this condition, as they place stress on their feet while moving side to side. Cuboid syndrome can often develop over time; however it can come out of a sudden injury as well. Over pronation, or other problems with feet, can exacerbate the condition if not corrected.
Among podiatrists, there is some disagreement about the treatment, as well as the definition of cuboid syndrome. Some see the injury as an injury to the ligaments located nearby the cuboid bone, while others believe it refers to the dislocation of the calcaneal-cuboid joint only. Treatment opinions differ as well. Although it can be treated by manipulation in order to reposition the bone, this must be done with extreme care in order to avoid injury. Some doctors, however, prefer treatment through the use of orthotic pads, designed to keep the bone in its place. Effectiveness of these treatments may vary, according to the severity of the injury.
When you experience side foot pain, it is important that you seek medical assistance. If a subluxed cuboid is caught and treated early, treatment is usually successful, and individuals may begin activities such as sports when the pain subsides. If left untreated, the pain will worsen, and the condition could cause permanent damage.
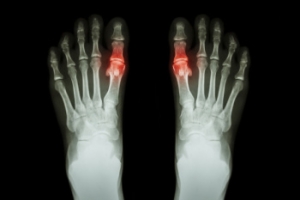
A Guide to Diagnosing Gout
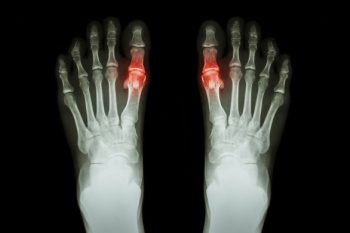
Gout, a form of inflammatory arthritis, can be excruciating, often affecting the big toe and ankles. Recognizing its symptoms is vital for timely management. The diagnosis begins with a keen observation of the symptoms, which are often sudden, intense joint pain, swelling, redness, and warmth, typically striking at night or in the early hours. The affected joint might feel tender to the touch, making even the lightest pressure unbearable. An accurate diagnosis often involves a comprehensive medical history review and a physical examination by a podiatrist. They may also conduct tests like joint fluid analysis to detect urate crystals, which are consistent with gout. Blood tests measuring uric acid levels can aid in confirmation, although high levels do not always guarantee a diagnosis. Imaging tests, such as X-rays, may reveal joint damage in chronic cases. If you have pain in the top of your foot, with a focus on the big toe, it is strongly suggested that you contact a podiatrist who can effectively treat gout.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Symptoms of Plantar Fasciitis

Plantar fasciitis occurs when the plantar fascia, a broad ligament that lies under the foot, becomes inflamed due to repetitive stress or strain. The hallmark symptom of plantar fasciitis is sharp, stabbing heel pain that can also radiate along the arch or sole of the foot. It typically worsens in the morning or after prolonged rest but often subsides with movement. Swelling and redness around the heel and arch area may accompany inflammation, and the affected area may feel tender or puffy. Stiffness and tightness in the foot can worsen throughout the day with increased activity. Discomfort in the foot's arch is also a common symptom of plantar fasciitis, limiting mobility and affecting daily activities. Pain and discomfort in the Achilles tendon may result from altered foot movement patterns caused by this condition. If you're experiencing any of these symptoms, it's suggested that you make an appointment with a podiatrist for a thorough evaluation and personalized treatment plan.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Treatment of Gangrene

For individuals with diabetes, the development of gangrene poses serious health risks and requires prompt treatment to prevent further complications. Gangrene results from necrosis, or death of body tissue in the lower legs and feet. Treatment for gangrene in diabetic patients involves a multifaceted approach aimed at halting tissue necrosis, controlling infection, and promoting wound healing. Surgical debridement is essential to remove any dead tissue and prevent further spread. Antibiotic therapy is used for managing bacterial infections associated with gangrene, often administered intravenously for severe cases. Restoring blood flow to the affected area through bypass surgery or angioplasty can help prevent tissue necrosis and reduce the need for amputation. Hyperbaric oxygen therapy delivers high-pressure oxygen to promote healing and control infection. Reconstructive surgery with skin grafts may be necessary to restore tissue integrity in extensively damaged areas. In severe cases, amputation may be required to prevent the spread of gangrene and facilitate prosthetic limb fitting. Throughout this treatment journey, podiatrists play a vital role in wound care, offering specialized expertise in diabetic foot care and wound management. If gangrene is a threat, it is suggested that you schedule an immediate appointment with a podiatrist for wound care and a prognosis.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Dangers of Falls Among Seniors

As you age, the risk of falls becomes a serious concern. Statistics reveal that more than one-fourth of older adults experience a fall each year. Many falls go unreported to doctors despite the doubled chances of falling again after the first incident. Falls often result in severe consequences, such as broken bones or head injuries that may compromise physical health and reduce independence. Contributing factors to falling include foot pain or wearing poorly fitting footwear. Additionally, lower body weakness, vision problems, and medication side effects can contribute to the risk of falls in older adults. To help prevent falls, seniors are encouraged to schedule appointments with a podiatrist to assess foot health, footwear, and gait abnormalities. Engaging in regular strength and balance exercises can help by improving stability and reducing fall risk. Regular eye exams and updating eyeglasses as needed can enhance visual clarity, especially for outdoor activities. Making the home environment safer by eliminating trip hazards, installing grab bars in bathrooms, and ensuring adequate lighting is also important in fall prevention. If you have injured your feet during a fall, it is suggested that you schedule an appointment with a podiatrist.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018